What Every Man Should Know About Long-Term Health
Prostate Wellness: What Every Man Should Know About Long-Term Health
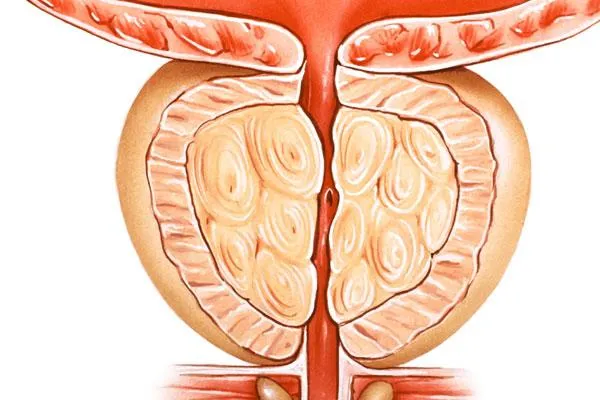
Prostate health is an increasingly important topic in men’s wellness, particularly as men age. The prostate, a small gland located below the bladder, plays a central role in reproductive and urinary function. Yet, many men overlook proactive steps to keep it healthy until symptoms arise.
In this article, we’ll explore what the science says about prostate wellness, consumer feedback on supplements and lifestyle changes, and practical strategies men can implement now.
Why Prostate Wellness Matters
Prostate enlargement (BPH): By age 60, more than 50% of men will experience benign prostatic hyperplasia (BPH), a non-cancerous enlargement of the prostate that can affect urination.
Prostate cancer risk: According to the American Cancer Society, about 1 in 8 men will be diagnosed with prostate cancer during their lifetime, making it one of the most common cancers in men.
Quality of life: Urinary difficulties, disrupted sleep, and reduced sexual function often impact daily living when the prostate isn’t functioning well.
The good news: nutrition, lifestyle, and evidence-backed supplements can all play a role in long-term prostate wellness.
What Science Tells Us — Prostate Wellness
Quick orientation
Prostate health research spans prevention of prostate cancer, management of benign prostatic hyperplasia (BPH, i.e., prostate enlargement), and symptom control (urinary frequency, nocturia, flow rate). Below we summarize mechanisms, human evidence, real-world caveats, and practical, safety-minded advice.
1) Diet & nutrients
Lycopene (tomatoes, watermelon, pink grapefruit)
Mechanism: Lycopene is a carotenoid antioxidant that can quench reactive oxygen species, modulate cell signaling, and influence androgen pathways that are relevant to prostate tissue biology.
What the evidence shows: Epidemiologic studies historically found inverse associations between lycopene intake (or tomato consumption) and prostate cancer risk, and some trials examined effects on PSA. Meta-analyses and randomized trials give mixed but suggestive results: some trials report small PSA reductions or slower PSA rise in men with higher baseline PSA, while other pooled analyses find no overall PSA reduction across all participants. This pattern—benefit in subgroups or early disease but inconsistent overall—means lycopene is promising but not definitive as a single preventive strategy. ScienceDirect+1
Practical takeaway: Encourage whole-food sources (cooked tomato products increase lycopene bioavailability). Typical dietary advice is safe: several servings per week of tomato-based foods (tomato sauce, tomato soup, cooked tomatoes) rather than relying solely on high-dose isolated supplements. Monitor PSA and discuss supplementation with a clinician if used therapeutically.
Zinc
Mechanism: The prostate normally accumulates high zinc concentrations which help preserve citrate production and regulate cell metabolism; zinc also participates in antioxidant defenses and apoptosis regulation. Low zinc status can disrupt these functions, potentially contributing to inflammation or dysregulated prostate cells. PMC+1
What the evidence shows: Reviews and mechanistic studies link altered zinc homeostasis with prostate disease. Human observational work finds lower serum zinc in some prostate cancer cohorts versus controls, but causality is uncertain. Clinical trials of zinc supplementation specifically for prostate disease are limited and mixed. PMC+1
Practical takeaway: Maintain adequate dietary zinc (oysters, beef, pumpkin seeds, legumes). Avoid very high supplemental zinc for long periods without medical advice (high doses can disrupt copper balance). Discuss zinc testing/supplementation with a clinician if there are deficiency concerns.
Omega-3 fatty acids (EPA/DHA)
Mechanism: Omega-3s modulate systemic inflammation, eicosanoid pathways, and cell membrane composition — all biologically plausible routes to influence prostate inflammation and tumor microenvironment.
What the evidence shows: Biomarker-based meta-analyses and cohort studies show inconsistent findings for omega-3s and prostate cancer risk: many studies show no clear increase or decrease in overall prostate cancer incidence when EPA/DHA levels are measured, though there are nuances by cancer stage and study design. For urinary symptoms and BPH, omega-3’s anti-inflammatory effects are mechanistically supportive but clinical evidence is not robustly conclusive. PubMed+1
Practical takeaway: Eating fatty fish 1–2 times per week (or a clinician-recommended algae/ fish oil supplement) supports general cardiovascular and inflammatory health and is reasonable as part of a prostate-healthy diet. Don’t expect omega-3s alone to prevent prostate cancer; they are one element in a broader pattern.
Cruciferous vegetables / Sulforaphane (broccoli, kale, cauliflower)
Mechanism: Crucifers contain glucosinolates that convert to bioactive compounds like sulforaphane and indole-3-carbinol; these compounds can activate detoxification enzymes, modulate epigenetic marks, induce apoptosis in abnormal cells, and reduce oxidative stress and inflammation. PMC
What the evidence shows: Epidemiological studies have linked higher crucifer intake with lower prostate cancer risk. Clinical and early phase trials of sulforaphane-rich extracts show biological activity in prostate tissue (changes in biomarkers, modulation of PSA doubling time in some studies) though large definitive phase III prevention trials are not yet established. Mechanistic and early human data are encouraging. PubMed+1
Practical takeaway: Include multiple weekly servings of cruciferous vegetables (steamed or lightly cooked to preserve glucosinolate conversion) as a practical, low-risk dietary strategy with plausible benefit.
2) Supplements & botanicals
Saw palmetto (Serenoa repens)
What the evidence shows: Saw palmetto has been extensively studied for BPH symptoms. Older meta-analyses and many RCTs suggested modest improvements in urinary symptoms and flow in some studies, but larger modern rigorous trials have produced mixed or null findings. Overall, evidence indicates some men may experience symptomatic relief, but results are variable and preparation/formulation matters. Recent large trials and reviews have tempered earlier enthusiasm. Side effects are generally mild but product quality varies. PubMed+1
Practical takeaway: If men choose saw palmetto, prefer standardized extracts from reputable manufacturers, discuss use with a clinician (especially if taking other medications), and set realistic expectations—monitor symptoms and consider medical therapy when symptoms are moderate/severe.
Beta-sitosterol (plant sterol)
What the evidence shows: Systematic reviews find beta-sitosterol improves urinary symptom scores and peak urinary flow compared with placebo, with relatively low adverse events. Effects on objective measures are smaller than prescription drugs (alpha-blockers, 5-alpha-reductase inhibitors), but beta-sitosterol can be a reasonable option for men with mild symptoms or those seeking non-pharmacologic approaches. PMC+1
Practical takeaway: Consider beta-sitosterol as a symptomatic option for mild LUTS/BPH; check product composition and dosage (many studies use ~60–130 mg/day, but formulations vary). Avoid assuming it replaces medical therapy for significant obstruction.
Green tea extract (EGCG)
What the evidence shows: Green tea catechins (EGCG) have antioxidant and anti-inflammatory effects and have been tested in trials focused on men on active surveillance or at increased risk. Clinical data suggest possible protective effects and favorable biomarker changes; dosing and safety were evaluated in several phase II trials and ongoing studies. High-dose EGCG can have liver toxicity in rare cases, so clinical supervision is prudent for concentrated extracts. PMC+1
Practical takeaway: Regular green tea consumption is low risk and potentially beneficial. Use concentrated supplements cautiously and under medical guidance—prefer doses validated in clinical trials and from third-party-tested brands.
3) Lifestyle factors
Exercise
Evidence: Multiple observational studies and interventional data link regular physical activity—especially brisk walking and aerobic conditioning—with lower risk of clinically significant BPH and lower risk of prostate cancer progression and mortality. A large body of literature supports that improving cardiorespiratory fitness lowers incidence and progression risk. Even moderate activity (2–3 hours walking per week) correlates with measurable risk reduction. PubMed+1
Practical prescription: Aim for ≥150 minutes/week of moderate aerobic activity plus 2 sessions/week of resistance training. Improvements in fitness tend to track with better outcomes.
Weight management
Evidence: Higher BMI and central adiposity are associated with increased risk of BPH symptoms and with more aggressive prostate cancer in some cohort studies. Obesity promotes chronic inflammation, insulin resistance, and hormonal shifts that can accelerate adverse prostate outcomes. World Journal of Men's Health
Practical prescription: Weight reduction via sustainable diet and exercise lowers systemic inflammation and likely lowers risk for worse prostate outcomes; clinicians should incorporate weight counseling as part of prostate health care.
Alcohol & caffeine moderation
Evidence & mechanisms: Alcohol and high caffeine intake can irritate the bladder or increase urinary frequency and nocturia; some epidemiological analyses link high alcohol with mixed prostate cancer risk signals depending on pattern and dose. Reducing late-day alcohol and high caffeine intake can substantially relieve urinary symptoms associated with BPH. PubMed+1
Practical prescription: Limit evening alcohol and caffeine, track symptom response, and adjust intake if nocturia or urgency is present.
Consumer feedback & real-world notes
Men increasingly prefer combined strategies—diet + exercise + targeted supplements—rather than relying on a single “pill.” Surveys and market trends show demand for transparency, third-party testing, and clinically tested formulations. Product quality and variable supplement composition are common consumer concerns. New York Post+1
Bottom line — how to translate the evidence into practice
Diet first: Emphasize whole foods — cooked tomato products, cruciferous vegetables, fatty fish, nuts, and diverse plant fibers.
Target supplements judiciously: If used, choose standardized, clinically studied preparations (and discuss with a clinician).
Prioritize lifestyle: Regular aerobic and resistance exercise, weight management, and moderating evening alcohol/caffeine show consistent, low-risk benefits.
Screen appropriately: Follow guideline-based PSA/DRE screening timelines informed by age and family history; incorporate shared decision-making with a clinician.
Quality & safety: Use third-party tested supplements; avoid megadoses of single nutrients without testing or medical supervision.
Consumer Feedback & Market Insights
Men are increasingly proactive about prostate wellness — and it shows in consumer behavior:
Natural supplements are in demand. Saw palmetto, zinc, and lycopene-based supplements are among the top-selling men’s health products.
Transparency matters. Consumers want third-party testing, clinical references, and clear labeling on prostate wellness products.
Holistic approaches win trust. Men prefer multi-pronged regimens that combine nutrition, supplements, and lifestyle advice over “quick fixes.”
Surveys also reveal that men are more likely to purchase prostate health products if recommended by healthcare providers or supported by credible scientific studies.
Practical Prostate Wellness Strategies
Eat for prevention: Prioritize tomato-based foods, cruciferous vegetables, fatty fish, and nuts.
Supplement smartly: Look for clinically studied doses of saw palmetto (typically 320 mg/day) or beta-sitosterol.
Stay active: Incorporate both aerobic and resistance training into weekly routines.
Get checked: Regular PSA tests and digital rectal exams (DRE) after age 50 (or earlier with family history) are essential for early detection.
Hydrate wisely: Balance fluid intake, avoiding excess caffeine and alcohol that worsen urinary frequency.